Insulin Resistance
THE MOST COMMON CAUSE OF ABDOMINAL WEIGHT GAIN
There can be a strong hormonal component to abdominal weight gain. And in most people, that hormone is insulin. Specifically, I’m talking about insulin resistance. And if you think that sounds complicated and like maybe it doesn’t apply to you, I encourage you to keep reading.
Because insulin resistance is, in fact, very common.
And could be affecting you even if your doctor said your blood sugar is normal.
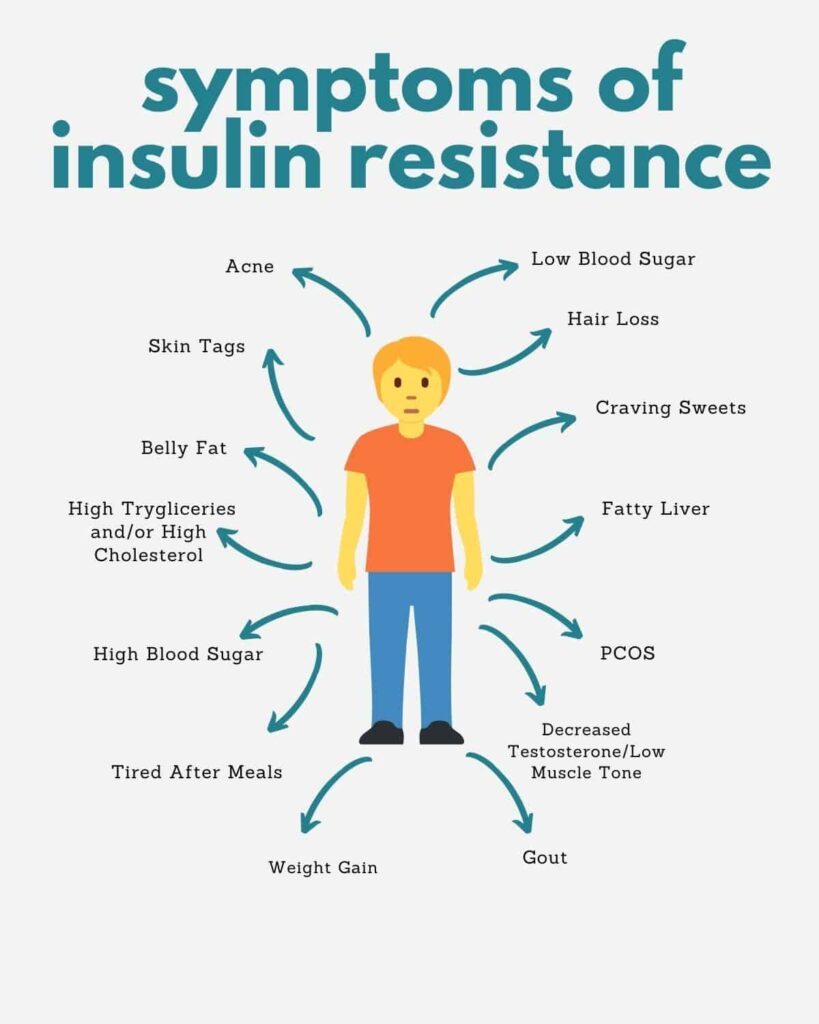
So let’s talk about insulin resistance which is also called hyperinsulinemia, pre-diabetes, or metabolic syndrome. And it’s common, affecting at least one in two people over 40. And lots of younger people. From a women’s health perspective, insulin resistance can play a major role in PCOS, of course, as well as the weight gain of perimenopause. Insulin resistance can make periods heavier and increase the long-term risk of heart disease, dementia, osteoporosis, and breast cancer.
So, it’s an important topic.
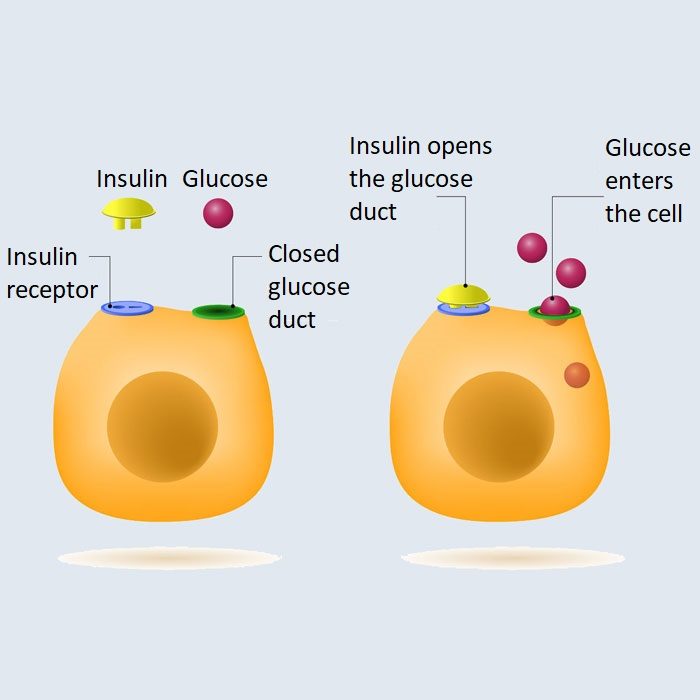
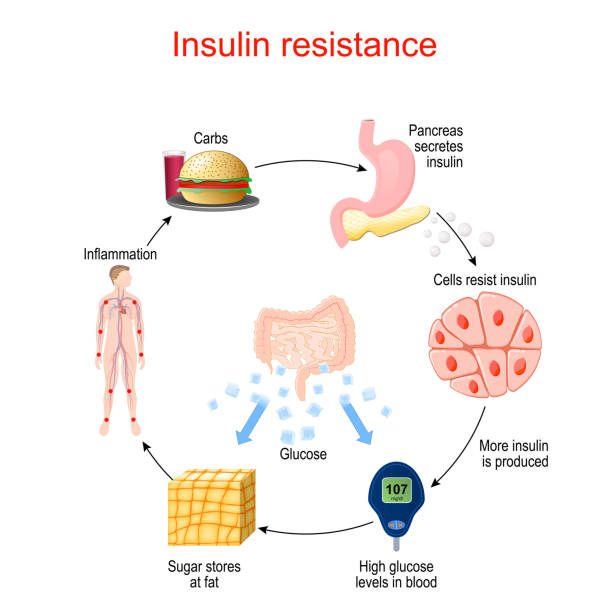
And let’s start with what is insulin resistance? In simplest terms, insulin resistance is dysfunction of the metabolic parts of the cell that are supposed to turn food into energy. The result of that metabolic dysfunction is less energy, more inflammation, and a greater tendency to gain fat, especially around the middle. Insulin resistance can also cause high cholesterol, high triglycerides and importantly, something called fatty liver (NAFLD – non-alcoholic fatty liver disease), which is fat accumulation in the liver. Actually, fatty liver is both caused by insulin resistance and a cause of insulin resistance.
So, if you’ve been told you have fatty liver, chances are high you do have insulin resistance, even if your doctor never mentioned it. Why would your doctor not mention insulin resistance? It could be that your doctor may suspect that you do have insulin resistance but holds the conventional view that insulin resistance is caused by weight gain.
And so, they skip over the insulin resistance part and just tells you to lose weight thinking that is getting at the source of the problem. In fact, growing evidence suggests that insulin resistance is not caused by weight gain but the other way around. In other words, weight gain, specifically abdominal or visceral weight gain, is caused by insulin resistance.
So. Being told to “just lose weight” to fix the underlying metabolic problem that is causing you to gain weight is putting the cart before the horse. A better approach is to identify insulin resistance, and then work to lower insulin, which will improve metabolic function and have the side benefit of creating weight loss around the middle.
How do you identify insulin resistance?
Signs of insulin resistance include, as mentioned, fatty liver, weight gain in the upper body and around the middle, skin tags, and another skin condition called acanthosis nigricans, which is a darkening of the skin in the armpits and around the neck. Now, just to be clear, you can have insulin resistance without having those physical signs but if you do have those physical signs, it’s very likely you have insulin resistance. Blood tests that suggest (but not diagnose) insulin resistance include high triglycerides and high cholesterol. Which of course, means that reversing insulin resistance can be an excellent way to lower cholesterol.
The liver enzyme ALT and another test called c-reactive protein (CRP) can be high with insulin resistance. And sometimes, blood glucose and hemoglobin A1C (or HbA1c) can be high. But quite often glucose and HbA1c are normal with mild to moderate insulin resistance. Which means that if your doctor only tested for glucose or HbA1c then she did not test for insulin resistance.
Instead, the test for insulin resistance is to test the hormone insulin. That can be done as a simple fasting insulin test, which just to say again, is different from a fasting glucose test. Then there is the glucose tolerance test with insulin. The glucose tolerance test with insulin is the test where you do a fasting blood test and then test again at 1 and 2 hours after a glucose drink. Except this time, you’re testing not just glucose but also the hormone insulin fasting and then at 1 and 2 hours after the glucose drink.
A healthy fasting insulin should be less than 10 mIU/L or 60 pmol/L. Depending on the units. One and two hours after the glucose challenge, a healthy insulin should be less than 60 mIU/L or 410 pmol/L. Of course, it’s normal for insulin to rise after the glucose challenge and after a meal. That’s its job. And insulin at the right level has many benefits including entraining circadian rhythm, building muscle, and if you’re a young woman, keeping your period going.
But insulin that is above those reference ranges—either fasting or peak insulin—is high insulin or insulin resistance and is a problem.
High insulin is both
1) a driver of weight gain, disease, and metabolic dysfunction, and
2) a biomarker of underlying metabolic cellular dysfunction.
But the good news is that it’s reversible. As insulin sensitivity improves, and insulin comes down, metabolic function is restored and weight loss can occur. In general, it’s probably not possible to lose much abdominal weight, or abdominal fat, until fasting insulin comes below 8 mIU/L, which can take several months depending on how high insulin was to start with. But the thing to understand is that you could be achieving significant metabolic improvement, Ie. reversing insulin resistance, for weeks or even months before you notice significant weight loss. Which means, you should not get discouraged if you don’t lose weight right away. As long as your insulin is coming down.
Insulin coming down means your metabolism is improving and you are setting yourself up for better health and future weight loss. You need to focus on improving something called metabolic flexibility. Which is the ability to switch between burning glucose and burning fat. Most of which happens in the mitochondria. Which are the little intracellular factories, or what I called the metabolic powerhouse, that turn glucose and fat into energy. And you have quadrillions of mitochondria which are constantly being replenished so there’s lots of opportunity to make more and healthier mitochondria.
The biochemical connection between mitochondrial dysfunction and insulin resistance is a little complicated but it’s basically that when the mitochondria are overwhelmed by energy excess or other insult, they signal the rest of the cell including the insulin receptor to stop responding to insulin. Thereby temporarily stopping the flow of glucose to the mitochondria and temporarily sheltering the mitochondria from the reactive process of energy production. It’s explained in a quite famous paper called: “Insulin resistance is a cellular antioxidant defense mechanism.”
This, of course, raises the question of what causes the mitochondrial distress and therefore insulin resistance in the first place? It’s a big question and the answer is lots of things including energy excess, or overeating. But lots of other things.
Other insults to mitochondria and insulin sensitivity include:
- environmental toxins,
- medications,
- ultra-processed food,
- circadian disruption,
- sarcopenia,
- nutrient deficiency,
- neuroendocrine issues,
- chronic inflammation, and
- microbiome issues
- just to name a few.
And all those metabolic insults seem to be having an epigenetic or transgenerational effect which means that each of the last two to three generations is more prone to insulin resistance than the generation before. Which means your insulin resistance is a negative effect of your environment and/or your parents’ or grandparents’ environment. And not necessarily something you’ve done wrong.
At the same time, you can still make changes to reverse insulin resistance and regain a healthy metabolism.
A full discussion of all the strategies would be a half day lecture. And this is just a bitesize blog. So, I’m going to have to just list some of my favourite strategies.
And of course, you don’t have to employ ALL the strategies at the same time, especially not all the supplements. It’s just a quick survey or overview of some of the things that can work.
Here we go. Effective, evidence-based strategies for reversing insulin resistance include:
- Moving the body to build muscle.
- Eating enough protein.
- Avoiding ultra-processed food.
- Fixing any underlying gut problems because meta-inflammation from the gut can cause or worsen insulin resistance.
- Supporting a healthy circadian rhythm with morning light and protein.
- Eating at the same time every day, which also helps circadian rhythm.
- Getting enough sleep.
- Reducing stress and enhancing parasympathetic tone and heart rate.
- Boosting oxytocin by, for example, getting a massage or spending time with friends.
- If you’re a woman, maintaining a good level of estrogen and progesterone, which enhances insulin sensitivity.
- And, if you’re a woman, not having too much testosterone, or not taking a progestin with a high androgen index, because too much testosterone can reduce insulin sensitivity.
- If you’re a man, the opposite is true. Too little testosterone can reduce insulin sensitivity.
Other strategies include:
- Gentle intermittent fasting, especially fasting overnight, which is called time-restricted eating.
- Supplements such as magnesium, taurine, myo-inositol, berberine, silymarin, and choline. Silymarin and choline work primarily by improving fatty liver, and that brings us to the strategy of avoiding high-dose fructose.
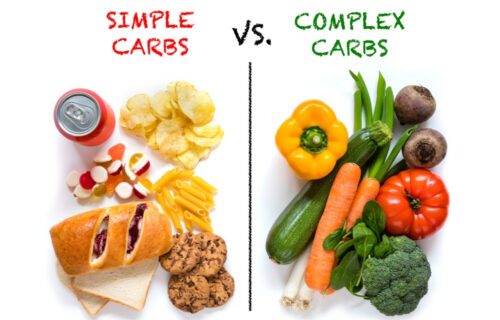
By which I do not mean fresh fruit, but am referring to concentrated high dose fructose from things such as soft drinks, fruit juice, and desserts, even natural desserts. At high dose, above a certain threshold (which is different for every individual) fructose spills over from the gut to the liver where it can cause mitochondrial damage, fatty liver, and insulin resistance. At a lower dose, most fructose is converted in the gut to glucose and organic acids. And is fine and healthy.
- A temporary low-carb or keto diet is another strategy, especially for more severe insulin resistance.
And finally, there are, of course, other non-insulin-resistance causes of weight gain which I’ll discuss in future blogs.