Joint Pain in Menopause
Causes of menopausal joint pain & how to ease it
Joint pain is one of the more common menopause symptoms and it can be one of the more debilitating as it reduces mobility and flexibility. I wanted to take a closer look at what causes joint pain in the menopause and how to treat and prevent achy joints through simple lifestyle and diet changes, natural therapies and supplements if needed.
Can menopause cause joint pain?
While aches and pains and joint stiffness are all common as we age, as women approach menopause, typically between the age of 45 and 55, many are often surprised to discover that joint pain is one of the most common symptoms, alongside hot flushes, night sweats, period changes and mood swings.
The average age for menopause is between 45 and 55, so it is little wonder why many women put their aches and pains down to aging.
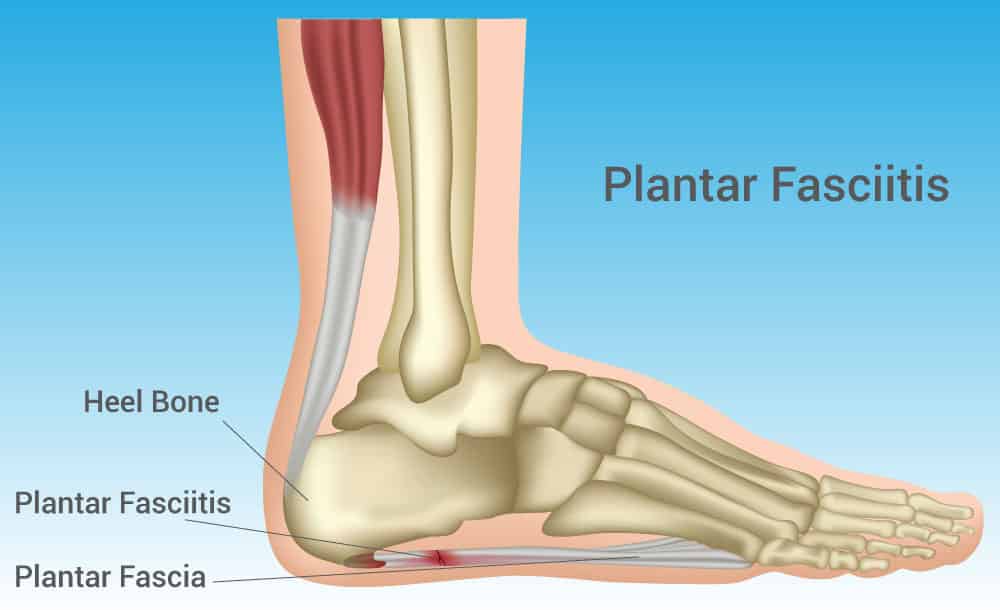
Joints which are involved in high impact movements such as the hips and knees tend to be most affected. The elbows, neck, shoulders, hands and fingers can also be affected by joint pain.
There are a number of causes of joint pain during menopause including:
- Hormonal changes
- Dehydration
- Stress
- Weight gain
- Diet
- Poor posture
- Increased sensitivity to pain.
Below, I take a closer look at each of these causes and recommend ways to help prevent and treat joint pain during menopause.
Hormonal changes
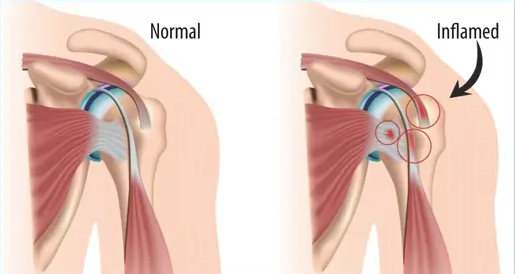
Falling oestrogen levels are thought to be one of the main causes of joint pain during menopause. As you reach menopause, levels of oestrogen in your body begin to drop. Oestrogen is responsible for regulating fluid levels in the body; therefore, if levels of this hormone are low, the body becomes less able to hold water, which can affect the hydration and lubrication of the joint tissues, including the cartilage, ligaments and tendons.
Up to 80% of cartilage is water,1 making it a very important component of this flexible and protective tissue, which acts as a cushion between the bones, absorbing shock and easing friction. Water is also a natural part of synovial fluid, a gel-like liquid which lubricates the cartilage and helps the joints move without creating friction.
Water is also needed to help support the flexibility and elasticity of the ligaments and tendons. Ligaments connect one bone to another and are needed for joint stability, while tendons connect your muscles to the bones. When your ligaments and tendons lose their elasticity, your range and ease of movement can be reduced.
Therefore, without enough water, the flexibility and lubrication of the joint tissues can all be affected. When this protective and supportive nature is impaired, it can cause aches, pains and stiffness to develop.
Fluctuating oestrogen levels may also give rise to underlying, low-grade inflammation as a result of the effects it has on the functions of joints, which could also be a factor in menopause joint pain.
Dehydration
Not drinking enough water and excessive sweating during menopause can also contribute to dehydration at this time. If you find that you experience joint pain and stiffness more in the morning, then dehydration during the night could be a contributory factor, especially if you are also experiencing night sweats.
Dehydration can also make it difficult for your kidneys to get rid of excess uric acid, which can cause a build-up of tiny, sharp crystals in and around joints, making them inflamed and sore.
Stress
Stress, surprisingly, can have a negative effect on your joint health. If you are experiencing a lot of stress, your body will release high quantities of the hormone cortisol. This hormone works as an inflammatory agent when present long-term, and so high levels of stress during the menopause will only make your joint pain worse.
Stress can also cause our muscles to tense up; this tension causes our joints to work so much harder which can lead to further inflammation and discomfort.
Weight gain
Excess weight puts additional pressure on weight-bearing joints such as the knees and hips.
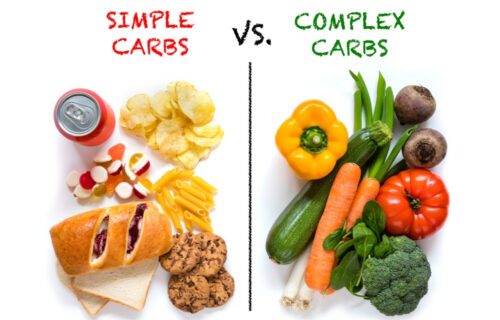
Unfortunately, weight gain is an all too common problem during menopause. Falling oestrogen levels can cause a problem with carbohydrate metabolism in some women, making it very easy to put on weight. Stress and lack of activity throughout the menopause can also cause weight gain.
Diet
Sugary foods, high-salt and processed food, as well as caffeine, fizzy drinks, and dairy can all trigger inflammation in the joints and aggravate joint pain.
There is also some debate about whether or not certain vegetables, known as the nightshade vegetables could exacerbate joint pain. Looking at what may be your trigger foods can make a huge difference.
Poor posture
Slouching puts extra pressure on your joints. It limits your range of motion and makes it so much harder for your muscles to take the load off your joints and, in time, it can cause misalignment of the spine which eventually leads to even more joint stress and pain.
Increased sensitivity to pain
Sleep issues are notorious during menopause and research has proven that sleep deprivation increases our sensitivity to pain: a study from the University of California found that sleep deprivation can change the circuitry in the brain in ways that amplify pain.3
Poor levels of essential nutrients are very common during menopause due to stress and digestive weakness.
What does menopause joint pain feel like?
Any of your joints can be affected, from little joints such as fingers and toes, right up to the major joints such as hips and knees.
Feeling achy, stiff and creaky and sometimes experiencing a burning feeling around the joints are typical symptoms of menopausal joint pain. These may be worse in the morning, improving as the day continues. While pain can be localised to individual joints or a few joints, many women also describe a feeling of aching all over.
How to treat menopause joint pain naturally
There are lots of simple and natural things you can do to help ease the discomfort of menopausal joint pain and to support your joint health. You should:
Drink plenty of water
Stay hydrated. Drink plenty of water to keep tissues moist and supple. In menopause, your body doesn’t retain water as well as it used to, so it’s important to replace the lost moisture. Water—not sports drinks, sodas, or coffee—is your best choice.
Strengthen your muscles & joints
Good options include:
- Non weight-bearing exercises (swimming, water aerobics and cycling)
- Low-impact weight-bearing exercises (walking, low-impact aerobics and dancing)
- Resistant, non-impact exercises (Pilates and yoga).
- Lift some weights – joint stability
- Strengthen your core – remember weakness in one part of your affects other parts
- Build in stretch breaks – especially if you are sitting for long periods
Eat foods that can help to ease joint pain
Reducing inflammation is a key part of reducing joint pain and improving overall joint health.
Some of the most beneficial anti-inflammatory foods include:
- Omega-3-rich foods
- Antioxidant-rich foods
- Other anti-inflammatory foods – Many fruit and vegetables have properties which reduce inflammation.
- And avoid foods that contribute to inflammation such as refined carbs like white bread and cake, fried foods, red meat and processed meats, soft and other sugary beverages, and foods with trans fatty acids like margarine.
Heat it up or cool it down
Heat, such as heating pads or warm baths, tends to work best for stiffness as it loosens and increases circulation.
Cold therapies such as ice packs can help to numb nerve endings, dulling pain and restricting blood vessels, slowing circulation and reducing swelling.
Try alternative treatments/therapies
Alternative treatments such as massage or acupuncture help many women with their joint pain symptoms. They directly target the area of pain in order to ease the symptom.
Correct your posture
The Alexander Technique can teach you how to hold your posture correctly and can be very effective at alleviating joint pain.
The best supplements for menopause joint pain
There are a number of supplements which can be beneficial in easing joint pain and supporting your joint health, such as vitamins, minerals and herbal remedies.
These include:
- Magnesium & calcium
- Vitamin D
- Omega-3
- Soy isoflavones
- Devil’s Claw
- Arnica
- Nettle
- Glucosamine
Keep tabs on your weight
Excess weight means excess pressure on your joints as you move, so losing even a few kgs (I know weight loss is tough during the menopause transition) can mean exponential relief for knees and ankles.
Destress.
I know, I probably sound like a broken record, but when it comes to joint pain, stress is especially problematic. Stress raises cortisol levels, and cortisol can cause additional inflammation in joints. Do what you can to keep stress in check. If stressed, consider taking a walk — in nature is best for a triple crown of stress- and joint-pain relief: nature, time away, and moderate exercise.
Conventional treatments for joint pain
Conventional medicines for joint pain include painkillers and anti-inflammatories. However, they are not usually recommended for joint pain associated with the menopause as the pain is a symptom rather than the cause itself.
Does menopause joint pain go away?
Most women do find that symptoms such as joint pain begin to ease off through the menopause as hormone levels even out and stabilise.
However, this can also depend on your general health, stress levels, diet, exercise etc. So looking after yourself well at this time is very important.
Is menopause joint pain the same as arthritis?
There are two main arthritic conditions: osteoarthritis and rheumatoid arthritis, and the onset of both of these conditions can coincide with menopause.
Osteoarthritis is a chronic (long-term) condition also known as ‘wear and tear’ arthritis. It typically starts with one or two joints, and the large weight-bearing ones such as the hips and knees are usually the first to become painful as the proactive cartilage wears away and is not replaced as fast as it is worn away.
Wear and tear is a natural part of ageing so most people will experience this to some degree. However, cartilage degeneration can be exacerbated or caused by other factors such as our genes, multiple pregnancies, poor diet, obesity, injury and overuse.
Osteoarthritis can be diagnosed by an x-ray which can show damage and other changes to the cartilage and joint tissues; whereas menopausal joint pain doesn’t cause the cartilage to breakdown and deteriorate in this way, therefore it wouldn’t show up on an x-ray.
While osteoarthritis typically occurs in older people due to wear and tear over the years, in contrast, rheumatoid arthritis is an autoimmune disease where the immune system starts to attack the tissues surrounding the joints.
This condition can be detected by a blood test and is usually episodic in nature, characterised by flare-ups of inflammation and pain and periods where symptoms are diminished. The joints of the hands and feet are most commonly affected, but other joints may be involved in severe cases.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5585083/
https://www.arthritis.org/living-with-arthritis/comorbidities/obesity-arthritis/fat-and-arthritis.php
https://www.jneurosci.org/content/39/12/2291
https://www.ncbi.nlm.nih.gov/books/NBK507245/
https://www.bmj.com/company/newsroom/acupuncture-may-ease-troublesome-menopausal-symptoms/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5783146/
https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/
https://www.ncbi.nlm.nih.gov/pubmed/20537472
https://academic.oup.com/rheumatology/article/57/5/798/4810410
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3580586/